Five Private Methadone Clinics in QLD Awarded PBS Numbers by The Minister for Health
In Australia, most medications are listed on the Pharmaceutical Benefits Scheme (PBS). This allows the government to subsidise the cost of everyday medications, providing affordable access for Australian citizens.
In the past, exceptions to this have existed, and one prominent example is Opioid Replacement Therapy (ORT) consisting of medications used to treat opioid dependence. For many years, private clinics have played a vital role in dispensing ORT medications outside of the PBS, providing vital care to thousands of Australians suffering from opioid addiction.
On July 1st 2023, the decision was made to list opioid replacement products such as liquid methadone, sublingual buprenorphine, buprenorphine/naloxone, and other long-acting injectables under the Highly Specialised Drugs section of the PBS schedule.
While this policy change was seen as a step forward for client access to Opioid Replacement Therapy (ORT), there was one blind-spot that had major consequences for public health.
In short, this policy change failed to consider that private addiction clinics were unable to supply medications listed under the PBS. As a result, private clinics would have been left unable to provide vital medications. These clinics, usually a medical centre co located with a dispensary, have traditionally provided care to a significant number of ODT patients across australia.
In order to remain in operation, private addiction clinics in South East Queensland applied to the Minister for Health, the honourable Mark Butler, for special approval to supply medications under the PBS.
On the 9th of May, 2024, the Minister approved their applications, and granted pharmacy numbers to five separate clinics in Southeast Queensland, ensuring continued access of vital ORT to their respective communities.
A Positive Policy Change with Unforeseen Challenges
The purpose of including methadone and other ORTs on the PBS schedule was to reduce the financial burden on those accessing these medications.
Under the new structure, patients could now pay a PBS co-payment of around $7.70 (for those with concession cards) or $31.60, instead of daily costs that could potentially exceed $200 per month.
However, while opioid replacement medication itself became more affordable, private clinics were no longer able to supply this to their patients, as they were operating outside the PBS framework.
As a result of this policy change, many clinics would have been forced to close their doors, leading to a potential crisis in opioid treatment access for a number of communities.
The Role of Private Clinics in Methadone Dosing
Private clinics were pivotal in providing methadone treatment, particularly for patients needing specialised care, supervised dosing, or support in managing their opioid dependence.
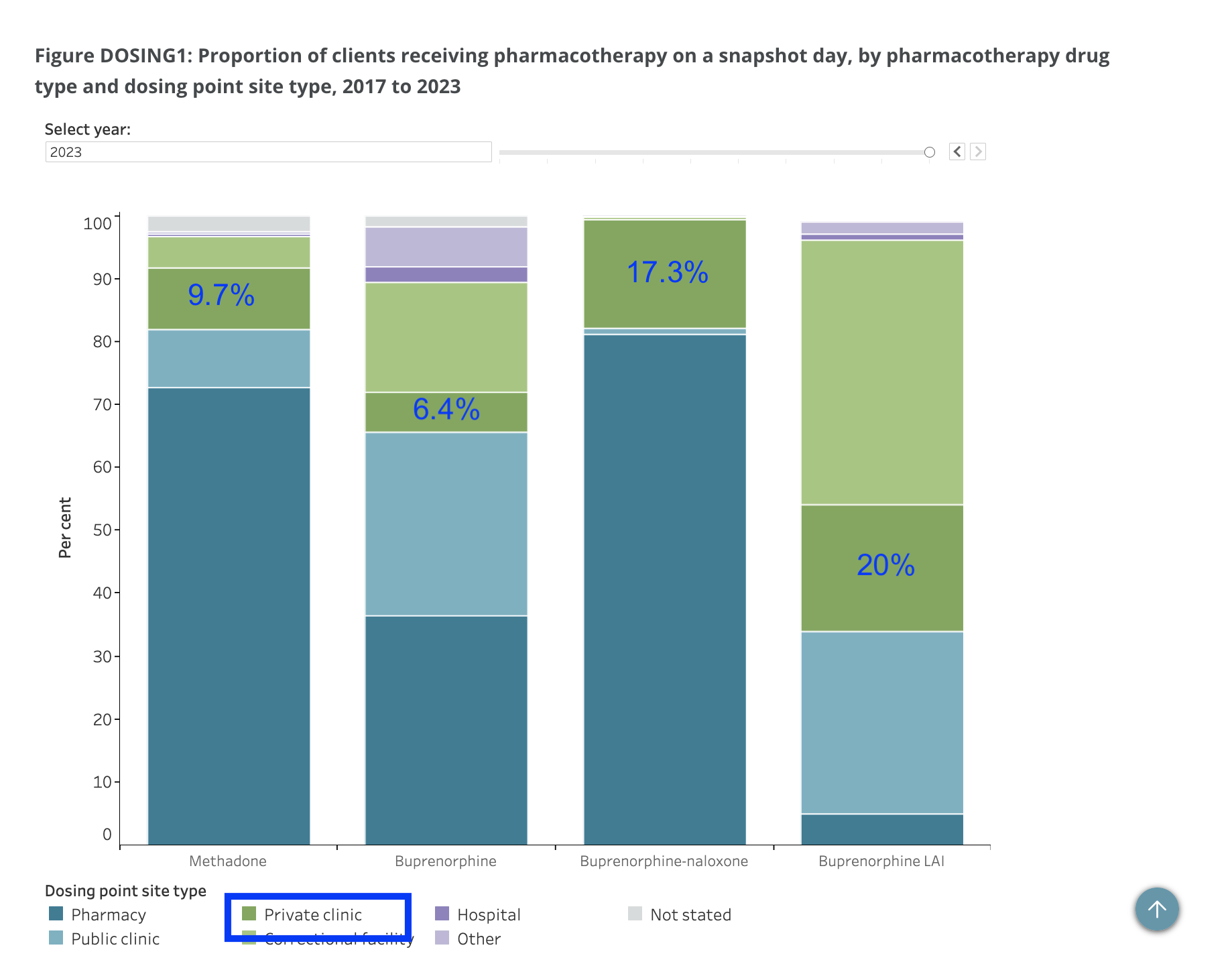
According to the National Opioid Pharmacotherapy Statistics Annual Data collection, on a “snapshot” day, about 2,515 patients (or approximately 9.7% of methadone patients nationally) received their treatment from private clinics.
With the inclusion of methadone to the PBS, these patients could have been left without access to consistent care if their local clinics were forced to close. The impact would have been particularly acute in areas like Southeast Queensland, where access to treatment was already a critical issue.
Ministerial Discretion: A Lifeline for Queensland Clinics
Due to this policy change, private clinics around Australia were forced to apply for approval to supply pharmaceuticals under the PBS. This prompted a lengthy legal process that took over 12 months to complete.
Matthew Frankland, co-owner of the private clinic Gold Coast Pharmaceutical Support (GCPS) on the Gold Coast, recalls the difficulties he faced during this uncertain period.
“In addition to potentially shuttering our Clinics effecting the livelihood of our Pharmacists, Doctors, Nurse Practitioners and Psychologis, I was very worried about my patients and the consequences for the community,” Mr. Frankland said. “There were many sleepless nights while we waited for a decision to come through.”
During this time, the fate of private clinics hung in the balance. Facing imminent closure, clinics in QLD worked closely with Queensland Health to develop a contingency plan, as almost 1500 patients could have lost access to their ORT.
Sarah Fenwick, Practice Manager at the private clinic Gold Coast Pharmaceutical Support, recalls the challenge of developing this contingency plan. As providing ORT as a service can be time consuming, it was a task community pharmacies were not equipped to deal with.
“I spent a day phoning every community pharmacy on the Gold Coast, to gauge their willingness to take on ORT patients,” Mrs Fenwick recalls. “I only found one pharmacy that was willing to take 2 patients.”
“We also explored the possibility of transferring these patients to the State Hospital system,” Mrs Fenwick said. “We quickly realised that this was not a viable option, as they were already under-resourced, and many of these patients require daily dosing.”
The only option left was for the Minister of Health to use their discretionary powers, provided under the National Health Act, to grant pharmacy numbers to these private clinics, allowing them to dispense PBS medications.
GCPS and several other private clinics approached the local Member of Parliament Angie Bell, to help advocate for their cause.
Mrs Bell, the Member for Moncreif, played a crucial role in campaigning for these private clinics in the Parliament. She petitioned the Minister for Health on several occasions to discuss the importance of keeping these private clinics in operation.
Recognising the potential fallout from this policy change, the Minister for Health, the hon Mark Butler, intervened using the discretionary powers granted under the National Health Act.
This allowed the Health Minister to grant PBS numbers to five private pharmacies in Queensland, enabling them to continue providing opioid replacement treatments under the PBS.
This decision has ultimately safeguarded access to care for thousands of patients who might have otherwise faced disruptions. It highlights the importance of maintaining continuity of care in opioid treatment, where stability is essential for positive outcomes.
Mrs Fenwick, along with many other employees in this sector, have been thrilled by the recent decision to be included under the PBS:
“Now that we have a PBS number,” Mrs Fenwick said, “we’re able to provide a better service to our existing patients, as we can provide access to all PBS therapies. Many of our patients have a number of comorbidities which we now have the capacity to support.”
The Minister’s use of discretionary power in this instance addressed a gap in the policy and helped prevent what could have been a significant public health issue.
The Human Impact: Voices from the Community
For many patients in Queensland, the availability of local, familiar treatment providers is a high priority. Opioid replacement treatment requires regular, often daily, supervision and support, which private clinics have consistently provided.
The transition to a system where only PBS-approved providers could offer ODT risked leaving patients without access to their trusted providers.
Patients, particularly those in Southeast Queensland, would have faced longer travel times and increased uncertainty in accessing their medication.
For a population already struggling with the challenges of opioid dependence, the prospect of such a disruption was a cause for alarm. Thankfully, the government took responsive action to prevent a potential crisis.
A Lesson in Adaptation
The inclusion of ODT on the PBS was intended to make life-saving medication more accessible and affordable for those who need it most. While it succeeded in reducing costs for patients, it inadvertently threatened the viability of many private clinics.
The Minister for Health's decision to grant PBS numbers to affected clinics in Queensland not only kept these crucial services running, but also highlighted the need for flexibility in policy-making.
As the healthcare landscape continues to evolve, ensuring that all patients (especially those with complex needs) have access to consistent, quality care should remain a priority.
This episode serves as a reminder that the path to better health outcomes often requires balancing big-picture reforms with the needs of those on the ground.